January is Glaucoma Awareness Month, strategically placed at the start of each new year to remind us to schedule our annual comprehensive eye exam because early detection is still the best way to prevent the irreversible vision loss that can be caused quietly in the early stages and without noticeable symptoms. According to Prevent Blindness, more than 2.8 million Americans age 40 plus have glaucoma and nearly half do not know they have the disease.
When it comes to glaucoma awareness, it’s always a good time to improve your understanding and evaluate your risk.
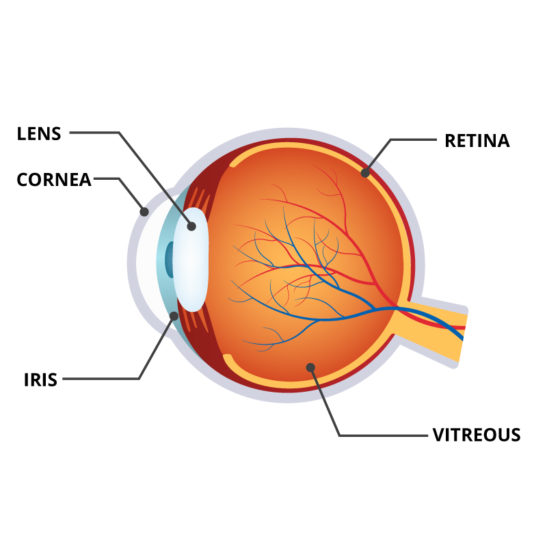
Glaucoma is an increased pressure in the eyeball. It can be thought of as a “plumbing problem” with either too much fluid entering a closed system or not enough fluid going out. The result is an elevation in the intraocular pressure. Over time the pressure will irreversibly damage the optic nerve, which sends visual information from the retina to the brain.
There are no overt symptoms, so the vision loss which begins peripherally can quietly progress unnoticed. Early detection is key to saving sight. Regular comprehensive eye exams are the best way to detect glaucoma in its early stages. Although there is no cure, there is effective treatment. Eye drops are commonly prescribed to control the pressure.
You are at a higher risk for developing glaucoma if you have a family history (especially a sibling), are of African, Asian or Hispanic descent; are over age 60, have diabetes or are severely nearsighted. If you are affected by any other eye disease it is also important to have your pressure tested regularly.

It should also be noted that pressure problems often occur after retinal procedures and may last for short or long periods of time. Dependent on individual patient anatomy or pathology, these pressure changes require careful and sometimes immediate attention if permanent damage to the optic nerve is to be curtailed or prevented. Pressure elevations may even occur long after retinal procedures, a result of “altered” slow changes in tissues over time. While everyone should be aware of the need to check their intraocular pressure on a routine basis, those having undergone a retinal procedure should be especially vigilant in the immediate postoperative period and periodically thereafter. Often slow elevations occur without noticeable symptoms.
Should you find yourself in any of the risk categories mentioned, please consult your ophthalmologist and be meticulous in keeping up with your exams to avoid visual impairment, legal blindness, and potentially even total blindness.

This article has been updated from original version published January 11, 2018.