If you have diabetes and develop any changes in your vision, contact your ophthalmologist immediately. While we currently do not have therapies that can completely reverse diabetic retinopathy (DR), we have effective treatments that can slow down or stop its progression and prevent your vision from further deteriorating. In some cases, therapies are effective at recovering some lost vision.
Therapies are employed to treat swelling of the central retina called diabetic macular edema (DME) and for treatment of severe DR that compromises blood flow to the retina.
Diabetic Macular Edema
If you are experiencing DME, your doctor might suggest injections into your eye with a medication known as anti-vascular endothelial growth factor (anti-VEGF) agents. These medications help to decrease the macular edema and improve vision. While the idea of a needle being inserted in your eye scares almost everyone at first, these therapies are highly effective and are in fact, a common procedure that retina specialists perform daily in their office. There are multiple anti-VEGF medications to choose from for diabetic macular edema. You should discuss with your retina specialist to determine which one is most appropriate for you.
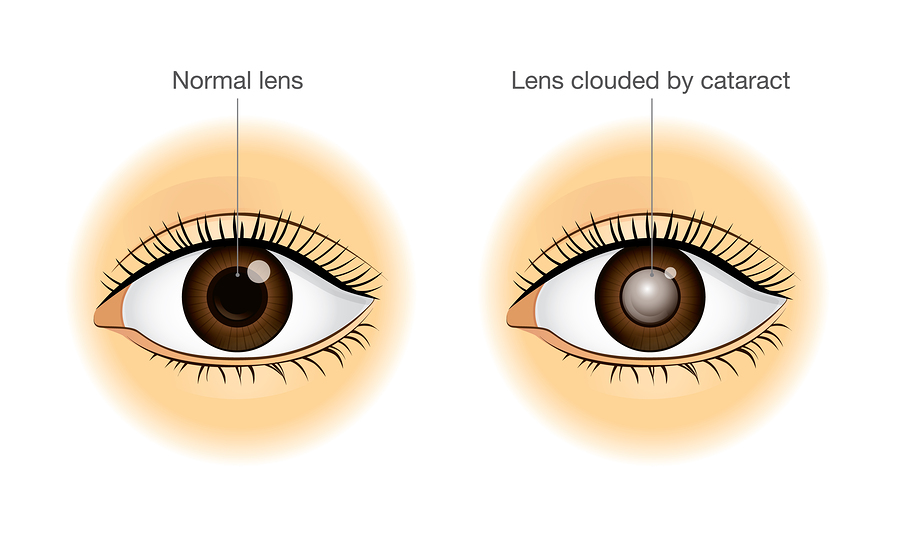
In some cases, your doctor might also recommend an injection into your eye of an anti-inflammatory medication known as a steroid. These injections may be suggested in patients that have had a prior cataract surgery and are experiencing worsening of their DME or have chronic DME despite treatment with anti-VEGF injections.
If the DME is just outside, but threatening to disrupt the central vision, your doctor may recommend a light focal laser to seal off the leaking blood vessels that are contributing to the retinal swelling.
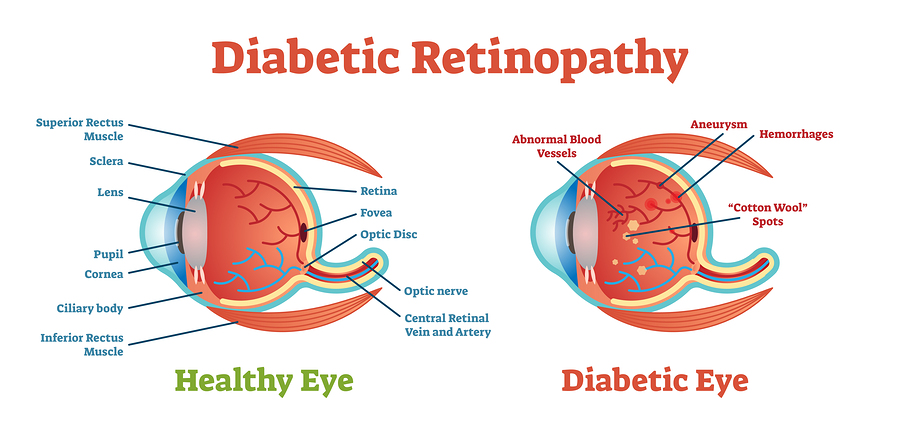
Severe Diabetic Retinopathy
If your DR results in a severe compromise of blood flow to the eye, your doctor may recommend a laser called panretinal photocogulation. This laser, while sometimes painful or uncomfortable, is remarkably effective in preventing total blindness from bleeding in the eye and retinal detachment.
If there already is blood in the eye, with or without scar tissue on the retinal surface, your doctor will likely recommend a surgery known as a vitrectomy to remove a gel-like substance inside your eye called the vitreous body. This procedure can also remove the bleeding and some of the scar tissue that has developed. These treatments are complex and visual recovery expectations need to be discussed with your treating retinal surgeon.
Recently, there has been growing evidence to support treatment of DR with anti-VEGF injections. While these treatments are effective, the frequency of treatments could pose compliance challenges for patients.
In conclusion, several management and treatment options are available for patients with diabetic eye diseases. Please consult with your doctor on the best management plan for you.
Written by:
Luis Martinez-Velazquez, MD, PhD will be starting his ophthalmology residency at Massachusetts Eye and Ear Infirmary.
Yasha Modi, MD is an Assistant Professor of Ophthalmology at New York University specializing in vitreoretinal surgery, retinal disease, and uveitis.